Immersive Learning for Medical Training: Virtual Surgeries and Diagnoses
Immersive Training Environments
Virtual reality (VR) is revolutionizing medical training, offering immersive environments that allow students to practice surgical procedures in a safe and controlled setting. These virtual operating rooms provide realistic simulations of complex anatomical structures and surgical instruments, enabling trainees to hone their skills without risking patient safety. This hands-on experience builds confidence and proficiency in a safe, repeatable environment, crucial for developing the precision and dexterity required in real-world surgical settings.
Realistic Anatomical Models
One of the significant advantages of VR in surgical training is its ability to create highly realistic anatomical models. These digital representations can be customized to depict various pathologies, injuries, and anatomical variations, offering a diverse range of scenarios for trainees to master. The detailed visualizations of complex structures, such as blood vessels and nerves, allow for a deeper understanding of the intricacies of the human body, fostering a more comprehensive understanding of the procedures they will face in practice.
Furthermore, the ability to manipulate and interact with these 3D models in VR allows trainees to explore different anatomical perspectives and visualize the surgical field from various angles. This level of interaction is essential for developing a thorough understanding of spatial relationships and surgical approaches.
Surgical Procedure Simulations
VR excels in providing realistic simulations of surgical procedures. Trainees can practice complex techniques like laparoscopic surgery, minimally invasive procedures, and open surgeries using virtual instruments and tools that closely mimic their real-world counterparts. The ability to repeat procedures virtually allows for focused practice on specific steps, fine-tuning dexterity and efficiency. This iterative feedback loop is invaluable in refining surgical skills and minimizing errors before engaging with real patients.
Haptic Feedback and Force Feedback
Advanced VR systems incorporate haptic feedback, allowing trainees to experience the tactile sensation of interacting with virtual surgical instruments. This crucial element enhances the realism of the simulation, providing a more intuitive and responsive experience. Force feedback systems further enhance this realism by providing resistance and feedback based on the virtual instrument's interaction with the environment, making the experience more akin to the physical reality of surgery. This precise interaction and feedback significantly enhances the learning experience.
Cost-Effectiveness and Accessibility
Compared to traditional surgical training methods, VR-based training offers significant cost-effectiveness. The need for expensive equipment and specialized personnel is reduced, making this technology more accessible to medical institutions and training programs worldwide. The ability to repeat simulations and customize scenarios without the need for live models or patients further amplifies the cost-effectiveness of VR in medical education. This accessibility empowers a broader range of learners and institutions to engage in high-quality training.

Affiliate marketing programs offer a powerful way for businesses to expand their reach and generate revenue by partnering with external websites or social media accounts. Understanding the essential principles of these programs is critical for success. Affiliate programs are essentially partnerships, where a company (the merchant) pays a commission to an individual or entity (the affiliate) for driving traffic and generating sales. This collaborative model allows both parties to benefit.
The Future of Medical Education: Embracing Innovation

The Integration of Technology
The future of medical education is undeniably intertwined with technological advancements. Interactive simulations and virtual reality (VR) are transforming how students learn complex procedures and anatomical structures. These immersive experiences allow for repeated practice in a safe, controlled environment, potentially leading to a more comprehensive understanding and increased proficiency in practical skills. This integration of technology also opens doors for personalized learning pathways, tailoring educational content to individual student needs and paces.
Furthermore, online learning platforms and digital resources are becoming increasingly crucial. These platforms facilitate access to a vast library of medical knowledge, enabling students to study at their own pace and engage with diverse perspectives. This accessibility is particularly important in bridging geographical gaps and making medical education more inclusive.
Personalized Learning Pathways
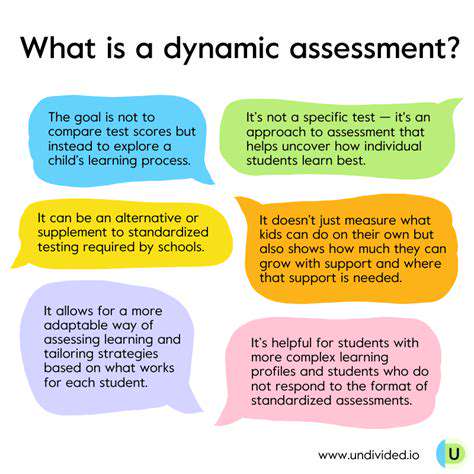
Moving away from a one-size-fits-all approach, personalized learning pathways are emerging as a key component of future medical education. This involves tailoring the curriculum and learning experience to individual student strengths, weaknesses, and career aspirations. Adaptable learning platforms and AI-powered systems will play a vital role in identifying individual student needs and providing customized learning materials and support.
By focusing on personalized learning, medical educators can foster a deeper understanding of complex medical concepts and promote a more engaged learning experience. This approach fosters critical thinking and problem-solving skills, allowing students to develop a personalized approach to patient care.
Emphasis on Interprofessional Collaboration
The evolving healthcare landscape necessitates a strong emphasis on interprofessional collaboration. Future medical education must equip students with the skills and knowledge to effectively collaborate with other healthcare professionals, such as nurses, pharmacists, and social workers. This collaborative approach is essential for delivering comprehensive and patient-centered care.
Integrating interprofessional learning experiences into the curriculum will foster a more holistic understanding of patient needs and promote a more effective approach to healthcare delivery. Simulation exercises and real-world case studies that involve diverse healthcare professionals will allow students to develop the communication and teamwork skills necessary for successful interprofessional collaboration.
Focus on Lifelong Learning and Adaptability
The rapid pace of advancements in medical science necessitates a focus on lifelong learning and adaptability in future medical education. Students need to be equipped with the skills to continuously update their knowledge and adapt to changing healthcare needs. This emphasis on lifelong learning is crucial for staying abreast of new treatments, technologies, and best practices.
Promoting a culture of continuous learning will empower medical professionals to engage in research, participate in professional development activities, and embrace new advancements in the field. This approach ensures that healthcare providers are well-prepared to meet the evolving challenges and opportunities in patient care.
Read more about Immersive Learning for Medical Training: Virtual Surgeries and Diagnoses
Hot Recommendations
- The Gamified Parent Teacher Conference: Engaging Stakeholders
- Gamification in Education: Making Learning Irresistibly Fun
- The Future of School Libraries: AI for Personalized Recommendations
- EdTech and the Future of Creative Industries
- Empowering Student Choice: The Core of Personalized Learning
- Building Community in a Hybrid Learning Setting
- VR for Special Education: Tailored Immersive Experiences
- Measuring the True Value of EdTech: Beyond Adoption Rates
- Addressing Digital Divide in AI Educational Access
- Preparing the Workforce for AI Integration in Their Careers